1. Distal radius: anatomical definition and structural overview
The distal radius forms the major articular surface of the wrist and contributes to both the radiocarpal joint and the distal radioulnar joint (DRUJ). The articular surface of the distal radius can be divided into two primary fossae:
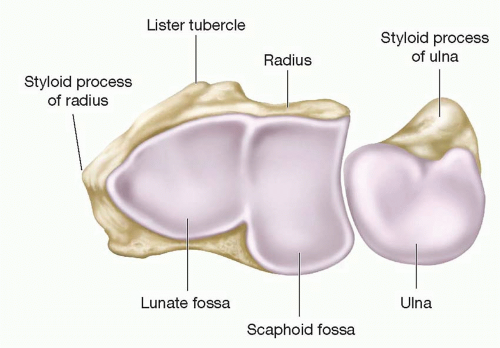
Scaphoid fossa:elliptical in shape and articulates with the scaphoid.
Lunate fossa: more spherical and articulates with the lunate.
Between these is a slight ridge. On the ulnar side is the sigmoid notch (ulnar facing), which forms part of the DRUJ and engages the distal ulna.
The metaphyseal region, 2–3 cm proximal to the radiocarpal joint, is composed predominantly of cancellous bone and flares to form the distal radial metaphysis. The volar cortex of the distal rad ius is thicker than the dorsal cortex, and the volar surface forms part of the floor of the carpal tunnel.
Important soft tissue structures: radiocarpal ligaments (radioscaphocapitate, radiolunate), triangular fibrocartilage complex (TFCC) on the ulnar side, dorsal and volar retinacular and capsular attachments; these influence fracture pattern and stability.
2. Radiographic parameters
Below are commonly used radiographic terms and short definitions used to quantify distal radial alignment.
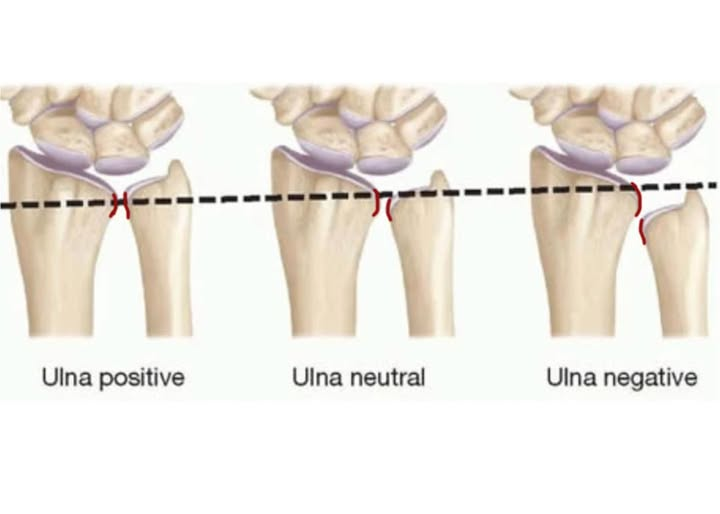
Ulnar variance: the relative length of the distal articular surface of the ulna compared with the radius, measured on a neutral PA radiograph.Ulnar variance affects load distribution across the wrist.
-Positive variance: When the ulna extends past the radius 1-4 mm. 4 mm is serious and needs surgical repair.
-Neutral variance: Ulnar and radial articular surfaces at the same level
-Negative: Ulna is relatively shorter than the radius
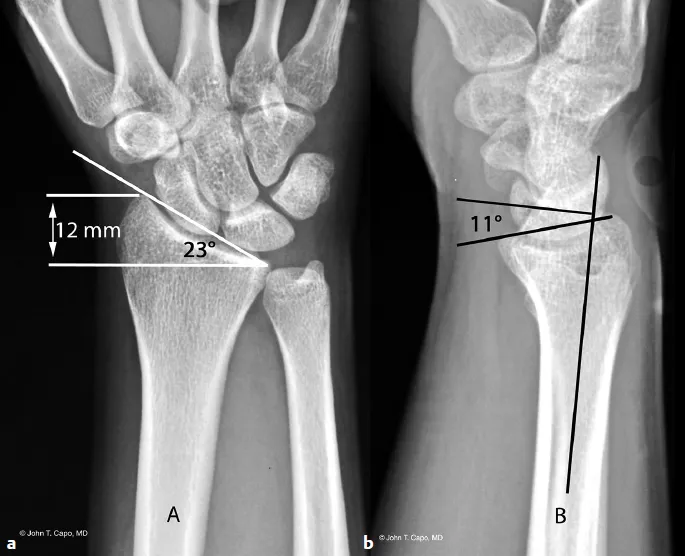
Volar tilt (palmar tilt): the angle formed on a true lateral radiograph between a line drawn along the distal radial articular surface and a line perpendicular to the longitudinal axis of the radius. Normal volar tilt is approximately 10–15° volar (palmar). Loss of volar tilt or dorsal tilt is clinically significant.
Radial height (radial length): measured on the PA radiograph as the distance from the tip of the radial styloid to the ulnar corner of the distal radius articular surface (or a consistent reference), usually ~11–12 mm in the normal adult.
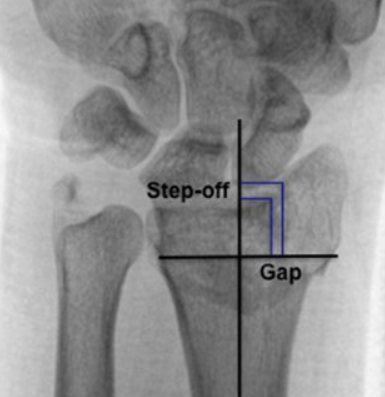
Intra articular step off and gap: direct measures of articular incongruity. Step off refers to a vertical displacement between adjacent articular surfaces; gap refers to a horizontal separation. A commonly used threshold for considering reduction inadequate is an articular step off or gap > 2 mm.
3.AO/OTA classification of the distal radius
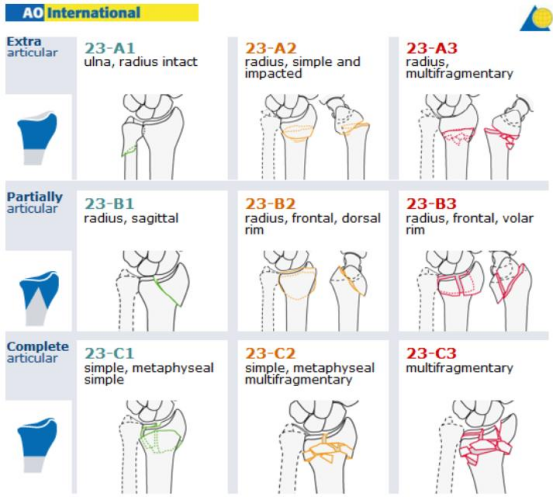
Type A — extra articular fractures
Type B — partial articular fractures
Type C — complete articular fractures (articular and metaphyseal involvement)
Each type is subdivided into groups (1–3) and subgroups; AO C3 denotes complete articular fractures with multifragmentary (comminuted) articular and metaphyseal components — the most complex AO distal radius category.
AO C3 (characteristics and challenges)
High degree of articular comminution with multiple small intra articular fragments.
Metaphyseal fragmentation often with bone voids / impaction.
Associated soft tissue injury and possible DRUJ involvement.
Reduction and stable fixation are technically demanding because small fragments may be difficult to capture with a single volar plate,achieving and maintaining anatomic articular congruity is critical.
CT imaging frequently clarifies fragment distribution and helps surgical planning in C3 fractures.
4. Common regions at risk for loss of reduction
Experience and series data (including case series of single VLP fixation) identify several fragments prone to secondary displacement:
1.Volar lunate facet (lunate fossa) fragments — loss of support here leads to collapse of the central articular surface and subsidence; this was the most common fragment to lose reduction in reported series.
2.Scaphoid fossa — central depression or settling causes step off in the scaphoid articular surface.
3.Radial styloid fragments — if not adequately reduced/fixed, can malrotate or subside
4.Mechanisms for loss of reduction
Inadequate initial reduction: articular impaction not adequately elevated or packed.
Plate positioning errors: plate placed too radially/proximally can prevent distal screws from supporting th
e lunate facet or may miss small volar fragments.
Insufficient screw purchase into small fragments: distal screw trajectory and length not optimized.
Bone loss / metaphyseal void: without graft or bone substitute, subsidence can occur.
Poor bone quality (osteoporosis): reduced holding power of screws.
Surgeons should pay special attention intraoperatively to confirm containment of the lunate facet and to assure the distal screw trajectory supports key fragments.
5. Surgical approaches: selection, schematics and advantages
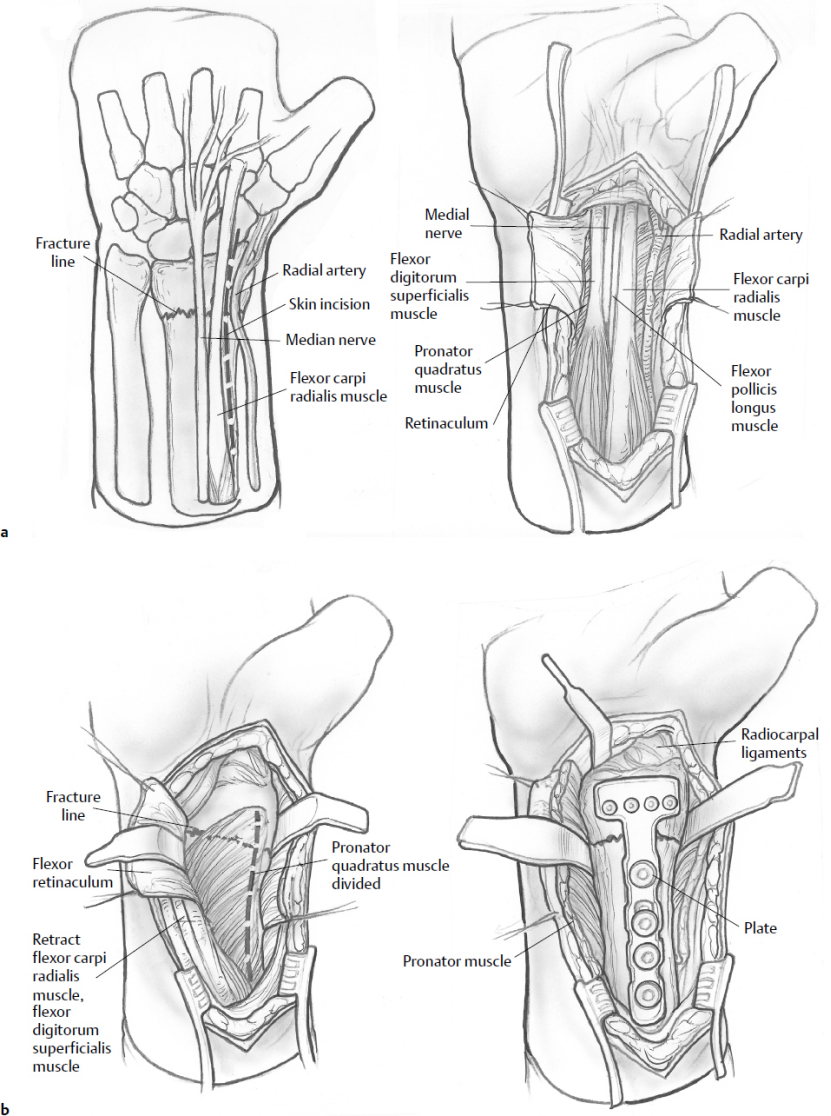
5.1 Extended Flexor Carpi Radialis (FCR) approach / Volar Henry approach
Indication: Most common volar approach for distal radius fractures; allows exposure of scaph
oid and lunate fossae and volar fracture fragments.
Technique highlights: skin incision centered over the FCR sheath, retract FCR and flexor tendons ulnarly, incise and reflect pronator quadratus to expose the volar distal radius. The extended FCR provides additional radial exposure toward the radial styloid. The modified Henry variant goes between FCR and radial artery.
Advantages:
Direct access to volar articular fragments (including volar lunate facet when sufficiently large), pronator quadratus provides a vascularized flap for plate coverage.
Lower risk of extensor tendon irritation compared with dorsal approaches.
Familiar exposure for applying volar locking plates.
Limitations:
Limited visualization of dorsal fragments; may not reach dorsally displaced / dorsal rim fragments.
5.2 Ulnar extensile approach to the distal radius
Indication: Volar ulnar corner fractures, access to sigmoid notch/DRUJ, volar ulnar comminution, or when DRUJ assessment/reconstruction is required.
Technique highlights: incision between ulnar neurovascular bundle and carpal tunnel contents; allows good visualization of the volar ulnar corner and sigmoid notch.
Advantages:
Direct access to the volar ulnar column and sigmoid notch, useful for addressing ulnar sided articular fragments and DRUJ pathology.
Limitations:
More specialized exposure; risk to ulnar neurovascular structures if not performed carefully.
5.3 Other considerations: dorsal approaches and combined exposures
Dorsal or dorsoradial approaches are useful when large dorsal fragments or dorsal rim comminution exist; dorsal plates or combined dorsal + volar constructs may be necessary for stability.
Combined approaches (volar + dorsal) sometimes required in severe C3 fractures to capture both volar and dorsal fragments.
6. LCP VOLALE DARLE Trabal ruptia प्लेट
Advantages
Fixed angle construct: locking screws create an angular stable construct that acts as an internal fixator and is less dependent on bone quality for distal fragment purchase.
Low profile on volar surface: compared with dorsal plates, reduced incidence of extensor tendon irritation.
Anatomic distal templates: many VLPs have distal screw holes oriented to support subchondral bone of lunate and scaphoid fossae.
Permits early motion: with sufficient fixation, patients can begin early wrist mobilization which benefits functional recovery.
Indications
Displaced distal radius fractures requiring ORIF where volar approach provides access to key fragments.
Many intra-articular fractures including some AO C3 fractures when fragments can be reduced and captured by the plate construct.
Osteoporotic fractures where locking screws aid fixation.
Contraindications
Extremely comminuted multifragmentary fractures where distal fragments are too small to be captured by the plate alone (eg, tiny volar lunate facets not amenable to plate screw purchase).
Large dorsal rim fragments that cannot be controlled via volar screws — may need dorsal fixation or combined plating.
Cases where plate positioning would inevitably impinge on tendon or joint if applied volarly.
7. Clinical outcomes
Overall success of single VLP in AO C3 fractures: retrospective series show maintenance of reduction to union in about 80–90% of cases when a single VLP is used and when plates are well positioned and fragments are adequately reduced.
Failure patterns: failures concentrate in cases with lunate facet involvement, inadequate distal screw support or plate malposition; some studies report loss of reduction rates from ~3–10% depending on case mix and definitions.
Comparative data: randomized and comparative studies show that combined fixation can offer better initial articular reduction in some highly comminuted patterns but may not yield superior long term functional outcomes and may be associated with higher hardware morbidity.
Note:The copyright belongs to the original author and the magazine,posts are for learning and communication only.