1. Introduction
Distal femoral osteotomy (DFO) is an essential surgical procedure for correcting angular deformities of the distal femur, commonly due to malunion, adolescent Blount disease, metabolic conditions, osteoarthritis, or idiopathic origins. These deformities significantly disrupt mechanical axis alignment, placing abnormal stress on knee cartilage and potentially accelerating the progression of osteoarthritis.
Over the past decade, two main fixation techniques have emerged for DFO: external fixation and internal fixation using locking plates. Both have been shown to offer accurate deformity correction, but which method delivers better outcomes for patients?
2.Comparing Internal and External Fixation Techniques
(A) External Fixation (Unilateral Frame)
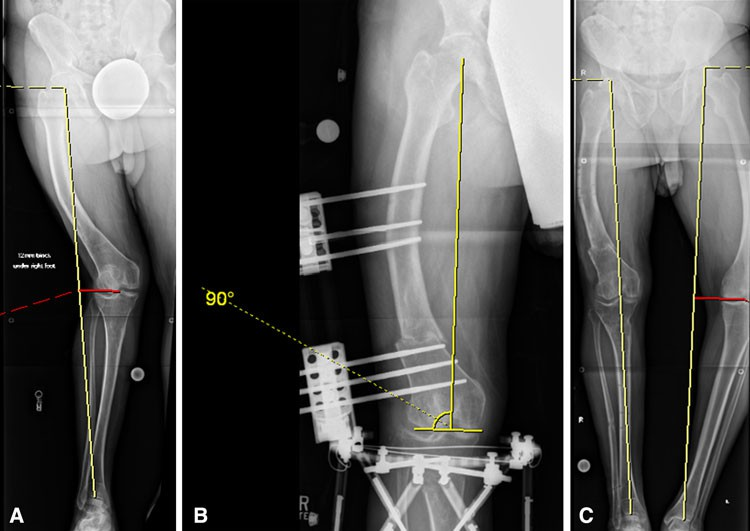
Fig. 1A–C The radiographs show the correction of deformity using a unilateral frame. The patient is a 48-year-old man with a marked windswept deformity. (A) A preoperative radiograph with a red line shows the MAD in the right limb. (B) This radiograph shows DFO and correction of the deformity with the unilateral frame. The yellow lines illustrate a normal LDFA of 90°. (C) A postoperative radiograph after removal of the unilateral frame is shown. The patient had a staged tibial osteotomy. MAD has been corrected to 0.
זעיר פולשני:
Entirely percutaneous, favorable in patients with thin thighs or when flexibility for postoperative correction is required.
Postoperative adjustability: External fixators allow gradual correction and are ideal for staged surgeries (e.g., femur and tibia).
Disadvantages:
Skin irritation and pin tract infections (reported in 6%–20% of patients).
Potential nonunion (9%–20%) and knee stiffness (up to 45%) in fracture treatment settings.
Aesthetic and psychological impact of wearing a frame for weeks or months.
(B) Internal Fixation(Fixator-Assisted Plating)
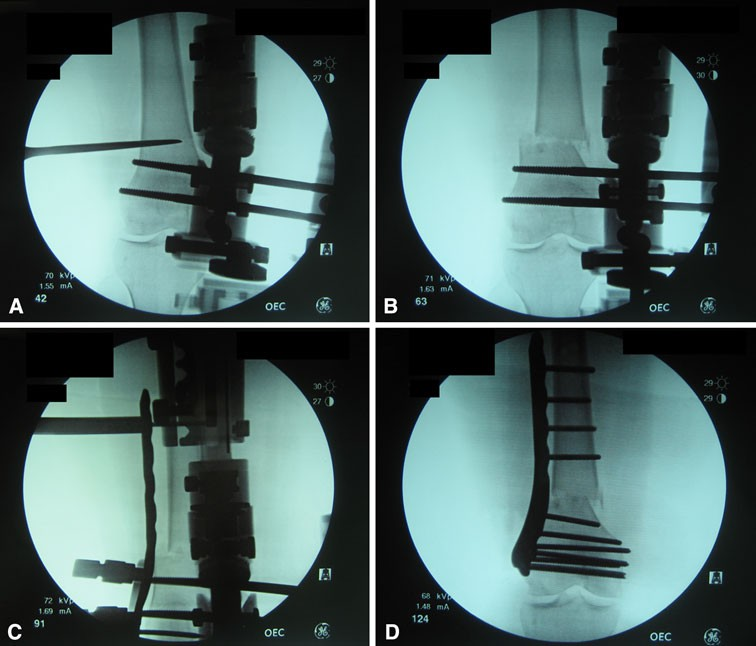
Fig. 2A–D The fluoroscopy images show the operative technique for fixator-assisted plating.(A) This image shows application of temporary frame and osteotomy, followed by (B) correction of deformity, (C) application of the lateral locking plate, and (D) plate fixation and frame removal.
Low-profile and rigid: Locking plates provide mechanical stability and avoid external hardware, allowing earlier mobilization.
Preferred for:
Patients with large thighs.
Those with adjacent implants (e.g., knee prosthesis).
Immunocompromised individuals who cannot tolerate external fixators.
Disadvantages:
Painful hardware (in 7 patients in a reviewed series), sometimes requiring plate removal after 10 months.
No option for postoperative angular adjustments.
Potential for bone loss under the plate and rare fixation failure.
3.Radiographic and Clinical Outcomes
Both methods achieved accurate correction of mechanical axis devi- ation (MAD) and lateral distal femoral angle (LDFA).
Intraoperative time was generally shorter with external fixation (due to fewer dissection steps).
Knee range of motion (ROM) and alignment outcomes were similar in both groups.
Complication profiles were overall lower in elective DFOs compared to trauma settings:
Locking plates: ~5% nonunion, ~5% fixation failure.
External fixators: increased risk of infection and nonunion in prolonged applications.
4.Conclusion
Both internal and external fixation techniques for distal femoral osteotomy provide accurate angular correction. The choice depends not just on the technical feasibility but also on patient preference, anatomical factors, and specific clinical scenarios.
Internal fixation offers greater comfort, earlier mobilization, and is now favored in many elective deformity correction centers. However, external fixation still holds value in complex, multi-level, or adjustable correction cases.
Ultimately, a shared decision-making process between surgeon and patient after transparent discussion of pros, cons, and expected outcomes is key to optimise results in DFO.